Platelet transfusion is often a necessity in the management of dengue hemorrhagic fever. Sometimes prophylactic platelet transfusion is also considered. However, despite clear guidelines about the indications of platelet transfusion, there is often a notable over-enthusiasm regarding the it, especially outside the government tertiary care hospitals.
Adapted from Dr Graham Beardsderivative work, CC BY-SA 3.0
Guidelines
Several guidelines regarding the management of dengue fever are in place which advise against unnecessary transfusion of platelet.
WHO Guideline
The 2009 guideline published by WHO is very conservative about platelet transfusion. It doesn't recommend prophylactic platelet transfusion at all. The guideline only recommends platelet transfusion in case of a massive bleeding uncontrolled by conservative methods.
In case of a hemorrhage, this guideline recommends using fresh packed red blood cells or fresh whole blood for resuscitation. If further blood loss occurs or haemodynamic status doesn't improve satisfactorily, then platelet transfusion can be consideredwho.
Indian National Guideline
NVBDCP guidelinenvbdcp suggests platelet transfusion under some situations. However they strongly discourage platelet transfusion when the platelet level is above 20,000/mm3.
The conditions under which platelet transfusion may be considered are as follows —
- In the absence of bleeding platelet transfusion may be considered when platelet count is below 10,000/mm3
- Prolonged shock with coagulopathy
- Systematic massive bleeding may require platelet transfusion in addition to packed red blood cells.
So in summary platelet transfusion may be considered if platelet count is below 10,000/mm3 or in case of massive bleeding and coagulopathy at any platelet count.
Literature
Guidelines are based on evidence after all, so let's take a look at the published literature.
Randomized Controlled Trial
A randomized controlled trial was performed in Lahorekhan in 2013 to evaluate effect of platelet transfusion in dengue. Eighty seven dengue patients were randomized to either receive platelet transfusion or no platelet transfusion. The median baseline platelet count was 10,000 and 10,500 respectively. Forty four percent patients in the treatment group had bleeding and 45% patients in the treatment group had the same. Almost half the patient in the treatment group responded to the platelet transfusion with an increased platelet count after transfusion. They also found that response was poorer in the patients having lower baseline platelet count. However, despite the increase in platelet count it didn't have any significant effect on either progression to bleeding or time to cessation of bleeding. However adverse reactions were associated with platelet transfusion including one death due to TRALI directly attributable to it.
A randomized controlled trial published in the Lancetlancet in 2017 randomized 372 dengue patients to treatment group with prophylactic platelet transfusion and control group with supportive care only. Eleven percent patient in the treatment group had either dengue hemorrhagic fever or dengue shock syndrome whereas 15% patients in the control group had the same. Clinical bleeding by day 7 or till discharge happened in 21% in the treatment group and 26% in the control group. The relative risk of bleeding was 0.86 (95% confidence interval 0.56 to 1.17) between the groups with a non-significant p value of 0.16. There were 13 adverse events in the treatment group and two in the control group which was statistically significant (p=0.0064).
Systematic Review
In 2017, a systematic reviewsysrev looked at all the prophylactic interventions for prevention of bleeding in dengue including platelet transfusion. They included 11 studies including the two randomized controlled trials mentioned earlier. They failed to find any relationship between platelet count and bleeding risk. Hence, prophylactic platelet transfusion is unlikely to have any role in preventing bleeding. On the other hand, platelet transfusion has significantly increased risk of adverse reactions.
Problems
There appears to be no benefit of prophylactic platelet transfusion in dengue. In fact overusing platelet transfusion has at least three serious consequences —
- Overuse of platelets strains the platelet reserve in the blood banks. Preparing a single unit of random donor platelet requires six units of whole blood. And about four to six units of platelets are usually transfused at a time. A single unit can only increaseplt platelet count up to 10,000/mm3. During an outbreak of dengue injudicious use of platelets would result in a crisis and the patients who actually require the platelets would be unable to get it.
- Platelet transfusion is associated with significant adverse reactions especially allergic complications. Fluid overload is also another concern in dengue patients. In the absence of any clear benefits, exposing the patient to these risks with prophylactic platelet transfusion seems unjustified.
- In an observational studytantock in Singapore it was found that the patients who receive platelet transfusion take longer to recover. In that study the recipients needed longer time for platelet to rise above 50,000/mm3 and their hospital stay was also longer compared to non-recipients which was statistically significant. Hence, unnecessary platelet transfusion may expose the patient to more harm than good.
Practice Gap
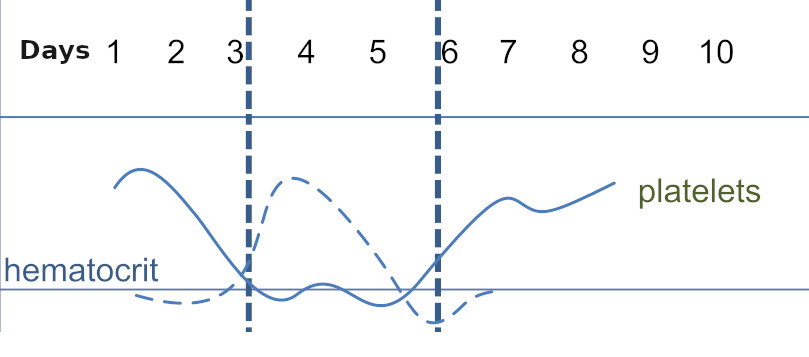
Despite clear evidence against prophylactic platelet transfusion there is significant gap between evidence and practice. The rapid fall of platelet count in the early phase of dengue often triggers a knee jerk response in the clinician to order transfusion of platelet. Even a tertiary care hospital in Delhi recordeddelhi a 23.2% inappropriate platelet transfusions in 2013.
In recent years even the patient parties are concerned about platelet and many of them demand transfusion of platelet without clinical indication. Considering the fragile doctor-patient relationship in India these days refusing such demands means risking unpleasant incidences in case of an unfavorable clinical outcome. In the end, the problem of platelet transfusion cannot be solved by individual clinicians alone, mass education and government intervention are also necessary.
- World Health Organization. (2009). Dengue guidelines for diagnosis, treatment, prevention and control : new edition. World Health Organization. https://apps.who.int/iris/handle/10665/44188 : page 42
- Directorate of National Vector Borne Disease Control Program. Guidelines for Clinical Management of Dengue Fever, Dengue Hemorrhagic Fever and Dengue Shock Syndrome. 2008. https://nvbdcp.gov.in/Doc/Clinical%20Guidelines.pdf : page 24
- Khan Assir MZ, Kamran U, Ahmad HI, et al. Effectiveness of platelet transfusion in dengue Fever: a randomized controlled trial. Transfus Med Hemother. 2013;40(5):362‐368. https://doi.org/10.1159/000354837
- Lye DC, Archuleta S, Syed-Omar SF et al. Prophylactic platelet transfusion plus supportive care versus supportive care alone in adults with dengue and thrombocytopenia: a multicentre, open-label, randomised, superiority trial. Lancet. 2017 Apr 22;389(10079):1611-1618. doi: 10.1016/S0140-6736(17)30269-6. Epub 2017 Mar 8. https://doi.org/10.1016/S0140-6736(17)30269-6
- Rajapakse S, de Silva NL, Weeratunga P et al. Prophylactic and therapeutic interventions for bleeding in dengue: a systematic review. Trans R Soc Trop Med Hyg. 2017 Oct 1;111(10):433-439. https://doi.org/10.1093/trstmh/trx079.
- Dipika Mohanty. Current concepts in platelet transfusion. Asian J Transfus Sci. 2009 Jan; 3(1): 18–21. https://doi.org/10.4103/0973-6247.45257
- Lee TH, Wong JG, Leo YS, et al. Potential Harm of Prophylactic Platelet Transfusion in Adult Dengue Patients. PLoS Negl Trop Dis. 2016;10(3):e0004576. Published 2016 Mar 25. https://doi.org/10.1371/journal.pntd.0004576
- Chaurasia R, Zaman S, Chatterjee K et al. Retrospective Review of Platelet Transfusion Practices during 2013 Dengue Epidemic of Delhi, India. Transfus Med Hemother. 2015;42(4):227‐231. https://doi.org/10.1159/000371500
 RSS Feed
RSS Feed
Write a comment: