Cryptococcal meningitis is a major cause of mortality in immunocompromised patients. The diagnosis of the condition requires a high level of suspicion and the management should be promptly started in order to save the patient.
Clinical presentation
An immunocompromised patient presenting with severe headache for some duration should raise the suspicion of cryptococcal meningitis.
The following clinical features may be expected in case of cryptococcal meningitisharrison —
- Headache
- Fever
- Cranial nerve involvement
- Visual deficits
- Neck rigidity may be present in some cases, but it is often absent in cryptococcal meningitis
Differential diagnosis
Other causes of meningitis must be excluded in patient suspected to have cryptococcal meningitis &mdas;
- Tubercular meningitis
- Bacterial meningitis
The major differentiating features of cryptococcal meningitis are as follows —
- Neck rigidity is often absent
- A somewhat chronic course of disease is seen which presents with headache of some duration
Diagnostic tests
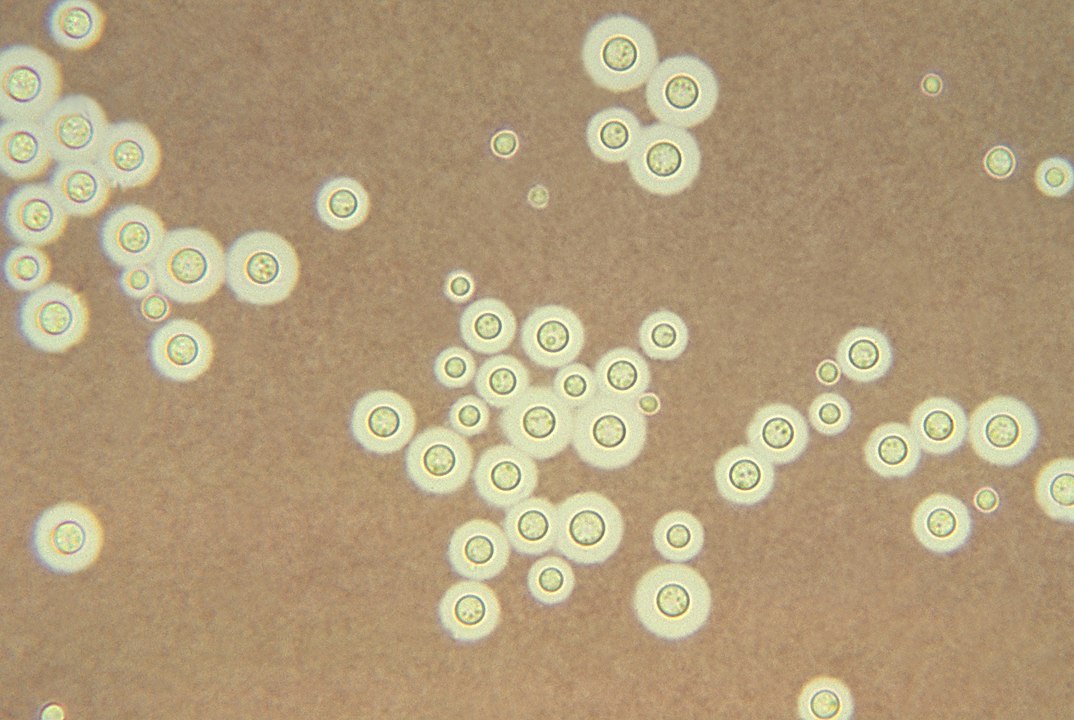
Any patient suspected of having cryptococcal meningitis should undergo a CSF study. During lumbar puncture the CSF often comes out in jet, so appropriate personal protection is warranted. The CSF sample should be sent for Indian ink preparation and fungal culture to establish the diagnosis of cryptococcal meningitis. CSF examination often reveals mononuclear cell pleocytosis and elevated protein level.
Serum and CSF cryptococcal antigen (CRAG) is an useful test to diagnose cryptococcal meningitis. It is both sensitive and specific and a positive result strongly suggests cryptococcal infection.Any patient with a positive serum CRAG, even without any symptoms, should undergo lumber puncture to exclude cryptococcal meningitis.crag
The following diagnostic tests should be done when cryptococcal meningitis is suspected to exclude other differentials —
- CSF study
- Cytology
- Protein and sugar
- Indian ink preparation
- Fungal culture
- ADA
- Gram stain
- Bacterial culture and sensitivity
- CSF CRAG
- Serum CRAG
Management
The management of cryptococcal meningitis requires medical as well as supportive cares.
Medical management
Medical management of cryptococcal meningitis involves three phases — induction phase, consolidation phase and maintenance phase. Management differs slightly between the settings where flucytosine available and where fluconazole is used instead5cVfluco.
| Phase | With flucytosineharrison | With fluconazoleambflu |
|---|---|---|
| Intensive phase | Amphotericin B (0.5-1 mg/kg) + flucytosine (100 mg/kg) daily for 2 weeks | Amphotericin B (0.75-1 mg/kg) + fluconazole (1200 mg) daily for 2 weeks or until CSF culture negative |
| Consolidation phase | Fluconazole (400 mg) daily for 10 weeks | Fluconazole (800 mg) daily for 6 weeks |
| Maintenance phase | Fluconazole (200 mg) daily | Fluconazole (200 mg) daily |
Maintenance phase is continued lifelong or until the absolute CD4 count is >200 cells/μL in at least 2 instances.
Patients without HIV do not require the maintenance phase.
In patients with renal impairments liposomal amphotericin B may be used in place of conventional amphotericin B.
Supportive management
Each patient of cryptococcal meningitis should undergo repeated therapeutic lumbar puncture to relieve the CSF pressurelp. Placing CSF shunt is also a viable alternative.
Ophthalmological examination should also be done to rule out papilledema.
Prognosis
Without treatment cryptococcal meningitis is always fatal. But even with treatment this disease carries poor prognosis.
Poor prognostic indicators areharrison —
- Indian ink positive for fungal elements
- High CSF pressure
- Low CSF glucose level
- Low CSF pleocytosis (<2 cells/μL)
- Recovery of yeast cells from extra-neural site
- Absence of capsular polysaccharide antibody
- CSF or serum CRAG > 1:32
- Concomitant glucocorticoid therapy or hematologic malignancy
Immune reconstitution inflammatory syndrome
Immune reconstitution inflammatory syndrome (IRIS) may happen with cryptococcal meningitis when there is a improvement in host immune status after initiation of anti retroviral therapy (ART). Hence it is necessary to exclude cryptococcal meningitis before starting ART.
Links
- Jameson, Fauci, Kasper, Hauser, Longo, Loscalzo. Harrison's Principles of Internal Medicine. 20th Edition. 1526-1529
- Chen J, Zhang R, Shen Y, Liu L, Qi T, Wang Z, Mehraj V, Routy JP, Lu H. Serum cryptococcal antigen titre as a diagnostic tool and a predictor of mortality in HIV-infected patients with cryptococcal meningitis.HIV Med. 2019 Jan;20(1):69-73
- Yao ZW, Lu X, Shen C, Lin DF. Comparison of flucytosine and fluconazole combined with amphotericin B for the treatment of HIV-associated cryptococcal meningitis: a systematic review and meta-analysis. Eur J Clin Microbiol Infect Dis. 2014 Aug;33(8):1339-44
- Loyse A, Wilson D, Meintjes G, Jarvis JN, Bicanic T, Bishop L, Rebe K, Williams A, Jaffar S, Bekker LG, Wood R, Harrison TS. Comparison of the early fungicidal activity of high-dose fluconazole, voriconazole, and flucytosine as second-line drugs given in combination with amphotericin B for the treatment of HIV-associated cryptococcal meningitis. Clin Infect Dis. 2012 Jan 1;54(1):121-8.
- Rolfes MA, Hullsiek KH, Rhein J, Nabeta HW, Taseera K, Schutz C, Musubire A, Rajasingham R, Williams DA, Thienemann F, Muzoora C, Meintjes G, Meya DB, Boulware DR. The effect of therapeutic lumbar punctures on acute mortality from cryptococcal meningitis. Clin Infect Dis. 2014 Dec 1;59(11):1607-14.
 RSS Feed
RSS Feed
Write a comment: